A Seton Hall virologist called the risk of a COVID-19 outbreak on campus “unacceptably high” after a Health Services interview with The Setonian clarified the University's testing and tracing protocols.
Health Services’ most detailed explanation of its protocols yet comes in the wake of three residents testing positive for COVID-19 this fall semester. The newly clarified testing and tracing procedures explain who can be tested by Health Services and for what reasons.

Students who have been exposed to a known case of COVID-19 are to be quarantined and will be able to access testing upon request, especially if they are symptomatic, according to Director of Health Services Diane Lynch. Residents who are exposed will be sent to Ora Manor for two weeks of isolation.
“We’re going to ask [close contacts] to quarantine for fourteen days, and maybe we would consider testing, but it doesn’t have to happen,” Lynch said. “It’s really more up to the person themselves as to whether they would feel better about the testing part. If they have no symptoms, it’s more of an optional thing.”
Students who do not have a known exposure but are showing symptoms can also go to Health Services to be considered for testing.
“We would see them as if we were seeing them for any other visit and also consider other things they might have because the symptoms of COVID are not very specific, so maybe we would also look at testing them for strep throat or the flu, but we would certainly also consider testing them for COVID right now,” Lynch said. “Obviously, we have a low threshold level for testing people, but we also know when it’s best to test someone.”
Last week, the CDC — in a move some experts have called “bizarre” — announced new guidelines that only symptomatic individuals should be tested for COVID-19, despite knowledge that asymptomatic cases are a large driver of infections.
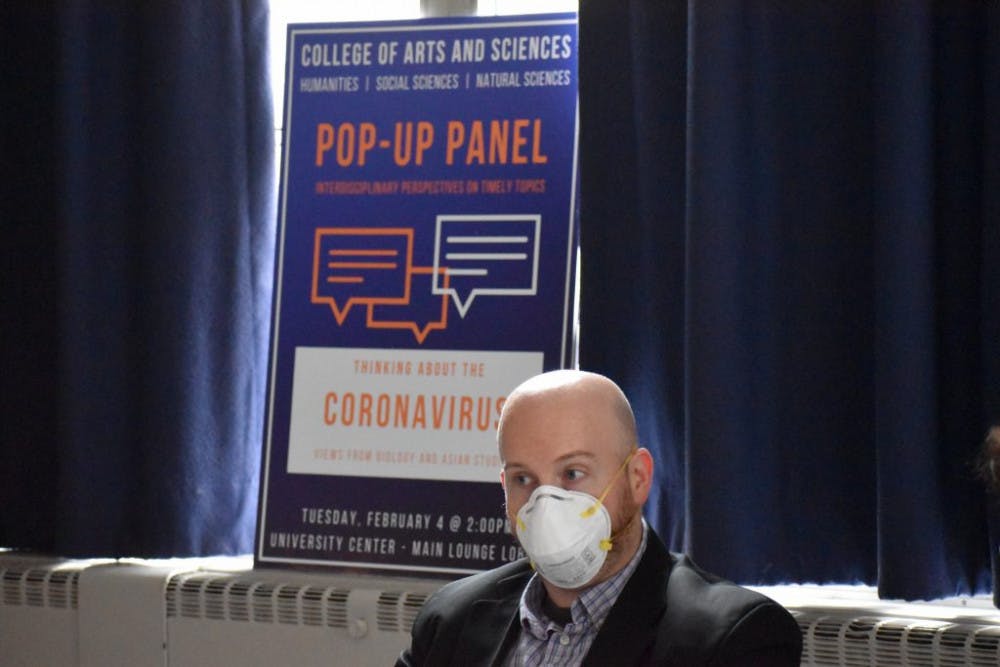
Dr. Brian Nichols, a virologist with a history of studying other coronaviruses like SARS-CoV-1, which prompted the 2003 SARS outbreak, and an associate professor of biology at Seton Hall says that the new guidelines do not go far enough.
“Now, all colleges can say they are following the CDC guidelines as the CDC only recommends testing symptomatic individuals,” Nichols, who has previously been cited by the University as an expert in how viruses spread, said. “However, most virologists question this guidance as it could have very dangerous consequences by allowing numbers of asymptomatic cases to rise on campus.”
“This is by no means me guaranteeing that we will have a significant outbreak as other campuses have had, but in my opinion, the risk is unacceptably high.”
According to the University’s website, the first positive COVID-19 case on campus this semester, announced on Aug. 15, was an asymptomatic individual. The University did not specify whether the other two cases that have been discovered on campus were symptomatic or asymptomatic.
Students who do not have clear symptoms and do not have exposure to a known case that lasted ten minutes or longer may not be tested by Health Services, according to Lynch.
“It would be like a strep throat test with no sore throat. It’s not going to be recommended, that’s for sure,” Lynch said of testing an asymptomatic individual with no known exposure. “Testing someone who has no known contact and no symptoms and no reason for getting the test… it has no meaning.”
Nichols, however, reiterated that asymptomatic people are a large driver of infections.
“Strep throat hasn't caused the U.S. to shut down and it certainly hasn't killed over 183,000 Americans since February,” Nichols said. “We should be testing and testing often.”
The University’s 69-page Restart Plan, which the state’s Office of the Secretary of Higher Education confirmed in July, requires quarantine for students with a known exposure and says all contacts and symptomatic individuals are “encouraged” to be tested.
“Seton Hall will encourage students who show symptoms of COVID-19 or have had known contact with someone who tested positive for the virus to get tested at Health Services,” the Plan, posted on the University’s website, says. “Contacts who develop symptoms should seek medical attention and get tested for COVID-19.
According to Lynch, testing asymptomatic individuals “doesn’t make a lot of sense and you’re using a resource that is a limited resource.”
However, she also said that there was no shortage of tests.
“We have probably 2,000 tests. Or more,” Lynch said, adding that more are on the way.
According to Nichols, that number is not enough.
“[This number of tests] ignores that we have a very large commuter population that is going into the classroom and interacting outside of it,” Nichols said. “Lack of regular testing is a flaw that creates an unacceptable risk.”
Lynch explained that insurance companies might not pay for tests they think are being given to low-risk individuals. In the wake of the new CDC guidance, that means unexposed asymptomatic people may not have their tests covered. It is not clear whether the University will pay for tests that insurance does not cover.
“Most of the time, if the testing is being done for what we would consider to be valid reasons, it should be covered by someone’s insurance,” Lynch said.
Concerning how students can access their results, Lynch explains that it depends on what kind of test the individual has received. Some students who came to live on campus from “high risk” states were given rapid polymerase chain reaction (PCR) tests, while other students were given standard PCR tests.
A “large number” of saliva tests, administered at move-in, were sent to a lab which “does not have an interface,” meaning results cannot be individually sent to the student via their student health portal. Other tests, such as the rapid tests, were sent to residents, Lynch said.
Students who need to access their results can call Health Services to receive them. Test results are currently taking about 48 hours to come back, according to Lynch.
In addition to testing, Nichols took issue with other parts of the plan’s implementation as well.
“Simply changing the HVAC systems isn't sufficient to fully address all the nuances of aerosol transmission,” Nichols said. “In addition, many of the physical barriers put in place are completely ineffective.”
“There's a lot of inadequacies with the current plan,” He said.
The University made a statement on the testing protocols on Wednesday.
“We recognize that experts throughout the nation have varying opinions about health care protocols and government policies designed to safely navigate the effects of the pandemic,” said University spokesperson Michael Ricciardelli. “The health and well being of our entire community remains our priority and continues to guide our planning and actions.”
Daniel O’Connor can be reached at daniel.oconnor1@student.shu.edu. Find him on Twitter @itsDanOConnor.





